Do you frequently experience a burning sensation in your stomach that rises to your chest, neck, and throat? Or perhaps you often have a sour or bitter taste in your mouth? These are some of the common symptoms of acid reflux, a condition that affects a large population. It’s important to spot and understand these symptoms, as acid reflux, also known as gastroesophageal reflux disease (GERD), can lead to serious complications if left untreated.
Table of Contents
ToggleIn this blog, we will explain what acid reflux symptoms feel like, what causes them, and how to manage them effectively. We’ll also talk about the dangers of ignoring them and when to seek medical help.
What is Acid Reflux?
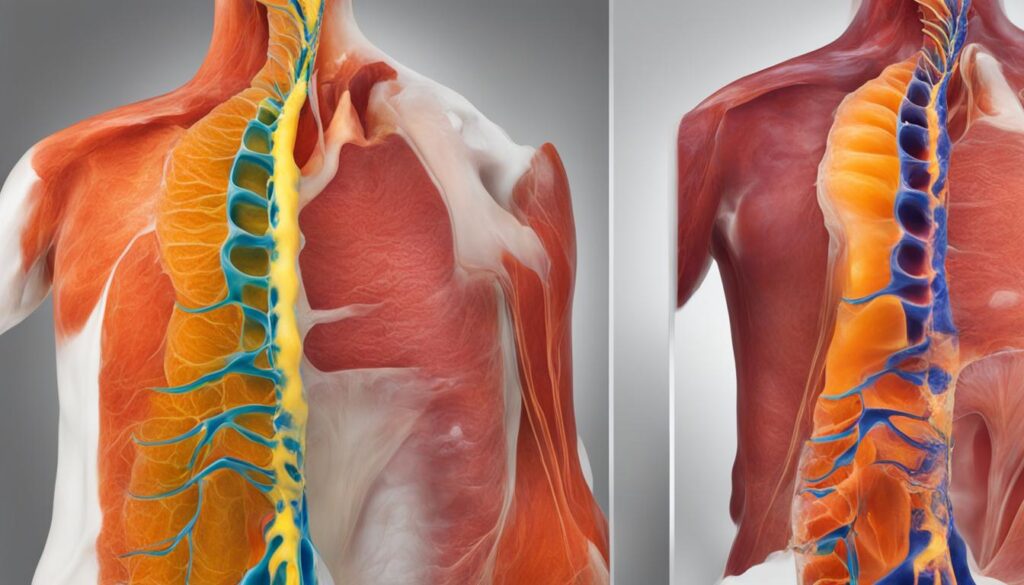
Acid reflux happens when stomach acid moves up into your food pipe, also called the esophagus. This acid is supposed to stay in your stomach to help digest food. But when it flows back, it causes discomfort, pain, and other symptoms.
What causes stomach acid to move up the esophagus?
When the muscle between your stomach and esophagus (called the lower esophageal sphincter or LES) gets weak or relaxes at the wrong time, acid can escape.
- Eating large meals or lying down after eating
- Obesity or pregnancy putting pressure on the stomach
- Smoking, which weakens the LES
- Drinking caffeine, alcohol, or carbonated drinks
- Eating fatty or spicy foods
When these triggers weaken your LES, acid reflux symptoms become more common and uncomfortable.
Is acid reflux the same as GERD?
Not exactly. Acid reflux is a condition. GERD (Gastroesophageal Reflux Disease) is a more serious, long-term form of it.
- Acid reflux can happen occasionally.
- GERD is diagnosed when reflux happens more than twice a week.
So while the two are related, acid reflux vs GERD symptoms can differ in how often and how severe they appear.
Symptoms of GERD
When it comes to gastroesophageal reflux disease (GERD), it’s important to be aware of the various symptoms that can occur. While persistent heartburn is the most common sign of GERD, there are other symptoms that you should watch out for.
Here are some of the symptoms that may indicate you have GERD:
- Feeling of fullness or lump in the throat: This sensation can make swallowing uncomfortable and may persist even after eating.
- Chronic cough: GERD can cause a persistent cough that doesn’t seem to go away, especially when lying down or after eating.
- Hoarse voice: If you find yourself frequently clearing your throat or your voice sounds raspy, it could be a symptom of GERD.
- Bad breath: The acid reflux from GERD can cause a foul odor in your mouth, leading to persistent bad breath.

Additionally, there are alarm symptoms that may indicate a more serious condition. These include:
- Difficulty swallowing: If you have trouble swallowing or feel like food is getting stuck in your throat, it’s important to seek medical attention.
- Pain when swallowing: Pain or discomfort while swallowing can be a sign of an underlying issue and should be evaluated by a healthcare professional.
- Nausea or vomiting: Frequent nausea or vomiting, especially after meals, can be indicative of GERD.
- Weight loss: Unexplained weight loss can be a cause for concern and should be discussed with a doctor.
- Anemia and bleeding: In some cases, GERD can lead to anemia or bleeding in the digestive tract, which requires medical attention.
If you experience any of these symptoms, it’s important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment.
What does acid reflux feel like?
Acid reflux symptoms feel different for everyone, but common signs include:
- Burning in throat or chest (heartburn)
- Sour taste in mouth
- Pain after meals or when lying down
- Regurgitation: food or acid coming back up
- Feeling bloated or full quickly
These are classic symptoms of acid reflux that shouldn’t be ignored.
Heartburn or heart attack?
Chest pain can be alarming, especially when you’re unsure of its cause. Heartburn and heart attacks are two conditions that can both result in chest pain, but it’s essential to understand the differences between them. Knowing the symptoms and seeking appropriate medical attention can help you identify whether you’re experiencing heartburn or a heart attack.
Heartburn is a common symptom of gastroesophageal reflux disease (GERD), which occurs when stomach acid flows back up into the esophagus. This upward movement of stomach contents can cause a burning sensation in the chest, often referred to as heartburn. Other symptoms of heartburn include:
- An acidic taste in the mouth
- Regurgitation of food or liquid
- Discomfort in the throat
On the other hand, a heart attack is a serious condition caused by reduced blood flow to the heart, leading to a lack of oxygen. The chest pain associated with a heart attack is typically more severe and intense than heartburn. Heart attack symptoms may include:
- Sudden onset of chest pain
- Pain that spreads to the arm, neck, jaw, or back
- Shortness of breath
- Feeling lightheaded or faint
How can I tell if chest pain is acid reflux or heart-related?
Chest pain from acid reflux symptoms usually:
- Happens after meals
- Gets worse when lying down
- Feels like burning or pressure, not stabbing pain
If you feel sudden or intense chest pain, seek help immediately. Never assume it’s just reflux.

What are the early signs of acid reflux?
Spotting the early signs of acid reflux can help prevent it from getting worse:
- Mild burning after eating
- Bitter taste in the throat
- Burping more than usual
- Mild chest discomfort
Catching these signs early can make treatment easier.
What are silent acid reflux symptoms?
Not all reflux feels like heartburn. Some people have silent acid reflux, which mainly affects the throat.
- Hoarseness or chronic sore throat
- Difficulty swallowing
- Feeling of something stuck in the throat
- Dry cough
These are common in people with acid reflux in adults who don’t feel the typical chest burn.
Symptoms in infants
Infants can also experience symptoms of gastroesophageal reflux disease (GERD). If you notice any of the following signs in your baby, it may indicate GERD:
- Frequent spitting or vomiting: Infants with GERD may spit up or vomit more often than usual.
- Refusal to eat: Difficulty in feeding or complete refusal to eat could be a symptom of GERD.
- Trouble swallowing: Babies with GERD may have difficulty swallowing or show signs of discomfort during feeding.
- Gagging or choking: If your baby frequently gags or chokes during or after feeding, it could be a sign of GERD.
- Wet burps or hiccups: GERD can cause wet burps or hiccups in infants.
- Irritability or arching of the back: Babies with GERD may become irritable or arch their backs during or after feeding.
- Weight loss or poor growth: Unexplained weight loss or inadequate weight gain could be a symptom of GERD.
- Recurring cough or pneumonia: GERD can cause a persistent cough or recurrent episodes of pneumonia in infants.
- Difficulty sleeping: Infants with GERD may have trouble sleeping, waking up frequently or experiencing discomfort during sleep.
If you suspect that your baby has GERD or any other health condition, it is important to consult a doctor for proper diagnosis and guidance.
Why is acid reflux common during pregnancy?
Pregnancy hormones relax the LES. Also, the baby pushes on the stomach.
- Common in 3rd trimester
- Feels like burning or bloating
These are normal but uncomfortable acid reflux symptoms.
How can symptoms be managed safely in pregnancy?
- Eat smaller meals
- Avoid spicy and acidic foods
- Sleep with head elevated
If needed, consult a doctor for safe medicines.

Causes of GERD
GERD, or gastroesophageal reflux disease, is often caused by the improper functioning of the lower esophageal sphincter (LES), a circular band of muscle located at the end of the esophagus.
Various factors can contribute to LES dysfunction, leading to the development of GERD. These causes include:
- Hiatal hernia
- Frequent consumption of large meals
- Lying down too soon after eating
- Smoking
- Being overweight or obese
- Pregnancy
- Connective tissue disorders
- Older age
- Anxiety
- Asthma
- Irritable bowel syndrome (IBS)
- Alcohol consumption
These factors weaken the LES or increase pressure on the stomach, allowing stomach acid and other digestive juices to flow back into the esophagus, causing the symptoms of GERD.
Dietary triggers
When it comes to managing GERD symptoms, paying attention to your diet is crucial. Certain foods have been identified as common triggers that can worsen acid reflux. By limiting or avoiding these foods, you can potentially reduce the frequency and severity of your symptoms.
Here are some foods that cause acid reflux:
- High-fat foods: Foods that are high in fat, such as fried foods and fatty meats, can relax the lower esophageal sphincter (LES), allowing stomach acid to flow back into the esophagus.
- Spicy foods: Spices like chili pepper, garlic, and onion can irritate the lining of the esophagus, triggering heartburn and other GERD symptoms.
- Pineapple and tomato: These acidic fruits can increase the acidity of the stomach, leading to acid reflux.
- Citrus fruits: Oranges, lemons, and grapefruits are highly acidic and can cause heartburn and irritation for individuals with GERD.
- Coffee and tea: Caffeinated beverages like coffee and tea can stimulate the production of stomach acid, worsening GERD symptoms.
- Carbonated drinks: Carbonated drinks, including soda and sparkling water, can contribute to acid reflux by increasing the pressure in the stomach.
By being mindful of these dietary triggers and making the necessary adjustments to your eating habits, you may be able to better manage your GERD symptoms. It’s important to remember that triggers can vary from person to person, so keeping a food diary and tracking your symptoms can help you identify your individual triggers.
Read: Foods to Avoid with GERD: What Not to Eat If You Have Acid Reflux

How Do Nighttime Acid Reflux Symptoms Affect Sleep?
Many people feel worse at night. That’s because lying down makes it easier for acid to travel up.
Why is acid reflux worse at night?
Gravity helps keep acid down during the day. At night, that help is gone.
- Lying flat lets acid escape
- Late-night eating increases acid production
- Poor sleep worsens digestion
This leads to nighttime reflux symptoms.
What are the signs of nighttime reflux?
Symptoms of nighttime reflux include:
- Burning chest pain in bed
- Coughing or choking at night
- Sore throat in the morning
- Trouble sleeping
These acid reflux symptoms affect sleep quality and daily life.
How can I sleep better with acid reflux symptoms?
Simple tips to improve sleep:
- Elevate your head 6-8 inches
- Avoid eating 2-3 hours before bed
- Wear loose clothes
- Sleep on your left side
These can lower acid reflux causes at night.
What tests are used to diagnose acid reflux symptoms?
Diagnosing gastroesophageal reflux disease (GERD) involves a comprehensive evaluation by a healthcare professional. It starts with a detailed medical history and a physical examination to assess your symptoms and their severity. Based on the information gathered, further tests may be ordered to confirm the diagnosis and rule out other conditions.
Diagnostic Tests
If alarm symptoms are present or if the diagnosis is unclear, your doctor may recommend additional diagnostic tests. These tests are designed to provide a more comprehensive understanding of your condition and help guide treatment decisions. Some of the common diagnostic tests for GERD include:
- Ambulatory 24-hour pH probe: This test measures the amount of acid in your esophagus over a 24-hour period. A small catheter is placed through your nose into the esophagus to monitor acid levels.
- Esophagram: Also known as a barium swallow, this X-ray test involves drinking a contrast material that coats the esophagus. The X-ray images can help identify abnormalities or structural issues.
- Upper endoscopy: This procedure involves inserting a flexible tube with a camera (endoscope) into your esophagus to visualize the lining and look for signs of inflammation, irritation, or other abnormalities.
- Esophageal manometry: This test measures the strength and coordination of the muscles in your esophagus. It helps assess the function of the lower esophageal sphincter (LES) and the movement of food through the esophagus.
- Esophageal pH monitoring: Similar to the ambulatory pH probe, this test also measures the acid levels in your esophagus. It involves placing a small catheter into your esophagus to monitor acidity over a certain period.
These diagnostic tests provide valuable information to your doctor and help determine the most appropriate treatment plan for your specific case of GERD. It’s important to follow your doctor’s recommendations and complete any necessary tests to ensure an accurate diagnosis.
Treatment for GERD
When it comes to treating gastroesophageal reflux disease (GERD), there are several options available that can help alleviate symptoms and improve your quality of life. A combination of lifestyle modifications and acid reflux treatment at home can often provide effective relief. In more severe cases, surgical interventions may be necessary.
Lifestyle Strategies
The first line of defense in managing GERD involves adopting healthy habits and making lifestyle changes. Here are some strategies to consider:
- Practice breathing exercises to reduce stress and promote relaxation.
- Include more reflux-friendly foods in your diet, such as lean proteins, whole grains, fruits, and vegetables.
- Maintain a moderate weight to avoid putting excess pressure on your stomach.
- Quit smoking, as it can worsen GERD symptoms.
- Avoid eating large meals before lying down and wait 2-3 hours after eating to lie down.
- Elevate the head of your bed during sleep to prevent stomach acid from flowing back into the esophagus.
Read: 5 home remedies for Acid Reflux and Gas
Medications
In addition to lifestyle modifications, your healthcare provider may prescribe medications to manage GERD symptoms. The following types of medications are commonly used:
| Medication | Description |
|---|---|
| Proton pump inhibitors (PPIs) | Reduce the production of stomach acid and help heal the esophagus. |
| Antacids | Provide immediate relief by neutralizing stomach acid. |
| H2 receptor blockers | Work by reducing the production of acid in the stomach. |
Surgical Interventions
In severe cases where lifestyle modifications and medications fail to provide relief, your doctor may recommend surgery to treat GERD. The most common procedure is called fundoplication, which involves wrapping the upper part of the stomach around the lower esophageal sphincter to strengthen it and prevent acid reflux.
Maintaining a healthy lifestyle, following your doctor’s recommendations, and sticking to your treatment plan can help manage GERD effectively.
Complications of untreated GERD
If left untreated, gastroesophageal reflux disease (GERD) can lead to various complications that can significantly impact your health. Here are some of the potential complications:
1. Esophagitis
Untreated GERD can cause inflammation of the esophagus, a condition known as esophagitis. This inflammation can lead to discomfort, pain, and difficulty swallowing.
2. Esophageal Stricture
Repeated exposure to stomach acid can cause the lining of the esophagus to become scarred and narrow, leading to a condition called esophageal stricture. This narrowing of the esophagus can make it difficult for food to pass through, causing swallowing problems.
3. Barrett’s Esophagus
Barrett’s esophagus is a condition where the lining of the esophagus undergoes changes, resembling the cells found in the intestines. This change in the lining can increase the risk of developing esophageal cancer in the long term.
4. Esophageal Cancer
In rare cases, untreated GERD can lead to the development of esophageal cancer. Esophageal cancer is a serious and potentially life-threatening condition that requires prompt medical attention.
5. Dental Problems
The chronic exposure to stomach acid can also have negative effects on your dental health. The acid can erode the enamel on your teeth, leading to tooth decay, sensitivity, and other oral health issues.
It is crucial to take steps to prevent, manage, and treat GERD to lower the risk of these complications. Consult with a healthcare professional to develop an individualized treatment plan that suits your specific needs and medical history.
Treatment options for occasional heartburn
If you experience occasional heartburn, there are various treatment options available to provide relief and help manage your symptoms. Here are some effective strategies:
- Over-the-counter antacids: Antacids are readily available without a prescription and can help neutralize stomach acid for temporary relief of occasional heartburn.
- Lifestyle changes: Making certain lifestyle changes can significantly improve your heartburn symptoms. Consider the following:
- Improving posture
- Maintaining a healthy weight
- Stopping smoking
- Eating more fiber
- Avoiding late-night meals
- Elevating the bed while sleeping
Making these changes may help reduce the frequency and severity of your occasional heartburn episodes.
For a visual representation of these treatment options, refer to the table below:
| Treatment Options | Benefits |
|---|---|
| Over-the-counter antacids | Provides quick relief |
| Lifestyle changes | Addresses underlying causes |
Implementing these strategies can greatly improve your quality of life by managing occasional heartburn effectively. Remember, it’s always a good idea to consult with a healthcare professional before starting any new treatment regimen.
Treatment options for frequent or severe acid reflux
If you are experiencing frequent or severe acid reflux, there are several treatment options available to help manage and alleviate your symptoms. Your healthcare provider may recommend the following:
- Prescription medications: Proton pump inhibitors (PPIs) and H2 blockers are commonly prescribed medications for acid reflux. PPIs work by reducing the production of stomach acid, while H2 blockers decrease the amount of acid released in the stomach. These medications can provide relief and help prevent the occurrence of acid reflux episodes.
- Alginate antacids: Alginate antacids form a protective barrier in the stomach, preventing stomach acid from backflowing into the esophagus. These antacids can help reduce the frequency and severity of acid reflux symptoms.
- Sucralfate acid suppressants: Sucralfate is a medication that adheres to the lining of the esophagus and stomach, creating a protective layer. This layer can help alleviate irritation and inflammation caused by acid reflux.
- Surgical interventions: In severe cases of acid reflux that do not respond to medications or lifestyle changes, surgical interventions may be considered. One common procedure is fundoplication, where the upper part of the stomach is wrapped around the lower esophageal sphincter to strengthen it and prevent acid reflux.
It is important to consult with a healthcare professional to determine the most appropriate treatment options for your specific condition. They can provide personalized recommendations and guidance based on your medical history and symptoms.
| Treatment Options | Description |
|---|---|
| Prescription medications (PPIs and H2 blockers) | Prescribed medications that reduce stomach acid production or decrease acid release in the stomach, helping alleviate acid reflux symptoms. |
| Alginate antacids | Antacids that create a protective barrier in the stomach, preventing stomach acid from flowing back into the esophagus and reducing the frequency of acid reflux episodes. |
| Sucralfate acid suppressants | Medications that adhere to the esophageal and stomach lining, creating a protective layer to alleviate irritation and inflammation caused by acid reflux. |
| Surgical interventions (e.g., fundoplication) | In severe cases where other treatments are ineffective, surgical interventions may be recommended. Fundoplication involves wrapping a part of the stomach around the lower esophageal sphincter to reinforce it and reduce acid reflux. |
By working closely with your healthcare provider and following their recommended treatment plan, you can find relief from frequent or severe acid reflux and improve your overall quality of life.
Get Expert Help for Your Acid Reflux Symptoms
If you’re dealing with ongoing acid reflux symptoms, don’t ignore them. Getting the right diagnosis and care can prevent long-term damage.
Dr. Nivedita Pandey, MBBS, Diplomate (Internal Med & Gastroenterology, USA), is a trusted and US-trained Senior Gastroenterologist and Hepatologist based in South Delhi. She specializes in digestive and liver disorders, including GERD, acid reflux treatment, obesity-related gut issues, and women’s health.
Book a consultation with Dr. Pandey today to take the first step toward relief and recovery.
FAQ
What are the symptoms of acid reflux?
The symptoms of acid reflux include persistent heartburn, a sour or bitter taste in the mouth, regurgitation of food or liquid, and alarm symptoms such as difficulty swallowing, pain when swallowing, nausea or vomiting, weight loss, anemia, and bleeding. Other symptoms may include a feeling of fullness or lump in the throat, chronic cough, hoarse voice, and bad breath.
How do I differentiate between heartburn and a heart attack?
Heartburn is caused by acidic stomach contents moving back up into the esophagus, resulting in a burning sensation. On the other hand, a heart attack is caused by reduced blood flow to the heart and may cause sudden, uncomfortable chest pain that can spread to other parts of the body. If you experience symptoms of a heart attack, it’s important to seek medical attention immediately.
What are the symptoms of acid reflux in infants?
Infants with acid reflux may experience frequent spitting or vomiting, refusal to eat, trouble swallowing, gagging or choking, wet burps or hiccups, irritability or arching of the back during or after feeding, weight loss or poor growth, recurring cough or pneumonia, and difficulty sleeping.
What causes acid reflux?
Acid reflux is commonly caused by the improper functioning of the lower esophageal sphincter (LES), which is a circular band of muscle at the end of the esophagus. Factors that can contribute to LES dysfunction include hiatal hernia, frequent large meals, lying down too soon after eating, smoking, being overweight, pregnancy, connective tissue disorders, older age, anxiety, asthma, irritable bowel syndrome, and alcohol consumption.
Are there any foods that can trigger acid reflux symptoms?
Yes, certain foods such as high-fat foods, spicy foods, pineapple, tomato, citrus fruits, coffee, tea, and carbonated drinks may trigger acid reflux symptoms. Limiting or avoiding these foods may help reduce symptoms.
How is GERD diagnosed?
A doctor will typically take a medical history and perform a physical examination to assess GERD symptoms. If alarm symptoms are present or if the diagnosis is unclear, further tests may be ordered, such as an ambulatory 24-hour pH probe, esophagram, upper endoscopy, esophageal manometry, and esophageal pH monitoring.
What are the treatment options for GERD?
Treatment options for GERD include lifestyle strategies, such as breathing exercises, consuming reflux-friendly foods, maintaining a moderate weight, quitting smoking, avoiding large meals before lying down, waiting 2-3 hours after eating to lie down, and elevating the head during sleep. Medications, such as proton pump inhibitors, antacids, and H2 receptor blockers, may also be prescribed. In severe cases, surgery may be recommended.
What are the complications of untreated GERD?
Untreated GERD can lead to complications such as esophagitis (inflammation of the esophagus), esophageal stricture (narrowing of the esophagus), Barrett’s esophagus (changes to the lining of the esophagus), esophageal cancer, and dental problems. It’s important to take steps to prevent, manage, and treat GERD to lower the risk of these complications.
What are the treatment options for occasional heartburn?
For occasional heartburn, over-the-counter antacids can provide relief. Lifestyle changes such as improving posture, maintaining a healthy weight, stopping smoking, eating more fiber, avoiding late-night meals, and elevating the bed while sleeping can also help manage symptoms.
What are the treatment options for frequent or severe acid reflux?
For frequent or severe acid reflux, prescription medications such as proton pump inhibitors (PPIs) and H2 blockers may be prescribed. These medications help decrease stomach acid production. Other treatment options include alginate antacids, sucralfate acid suppressants, and surgical interventions like fundoplication.
How can I manage and prevent acid reflux symptoms?
It’s important to recognize the symptoms of acid reflux, seek diagnosis and treatment from a healthcare professional, and make lifestyle changes to manage and prevent symptoms. With the right management and treatment, individuals with acid reflux can improve their digestive health and quality of life.
About The Author

Medically reviewed by Dr. Nivedita Pandey, MD, DM (Gastroenterology)
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist and hepatologist with extensive experience in diagnosing and treating liver diseases and gastrointestinal disorders. She specializes in liver enzyme abnormalities, fatty liver disease, hepatitis, cirrhosis, and digestive health.
All content is reviewed for medical accuracy and aligned with current clinical guidelines.





