Inflammatory bowel disease (IBD) is a chronic disease affecting the digestive tract. It has two types – Crohn’s disease and ulcerative colitis. These diseases can harm the colon and rectum, leading to symptoms that come and go. Flare-ups are often followed by times of no symptoms.
Table of Contents
ToggleIBD is an autoimmune disorder. Here, the body mistakenly attacks its own healthy digestive system tissues. Though its exact cause is a mystery, a mix of genetic, environmental, and immune issues contributes. People with a Jewish background or a family history of IBD are at higher risk. Even children, especially teens, can get inflammatory bowel disease.
Receiving a correct diagnosis and early treatment is key. This helps to manage symptoms, lower inflammation, and prevent serious issues such as colon cancer. By taking the right steps, you can handle your inflammatory bowel disease treatment. This can greatly enhance your well-being.
Understanding Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) covers two main diseases – Crohn’s disease and ulcerative colitis. These conditions cause ongoing inflammation in the digestive system. By learning about IBD, you can improve how you manage it.
What is Inflammatory Bowel Disease (IBD)?
IBD is an ongoing problem that causes swelling and irritation in the gut. It can lead to problems like stomach pain, diarrhea, and losing weight. What starts IBD isn’t known for sure, but it seems to involve genes, things in the environment, and your immune system.
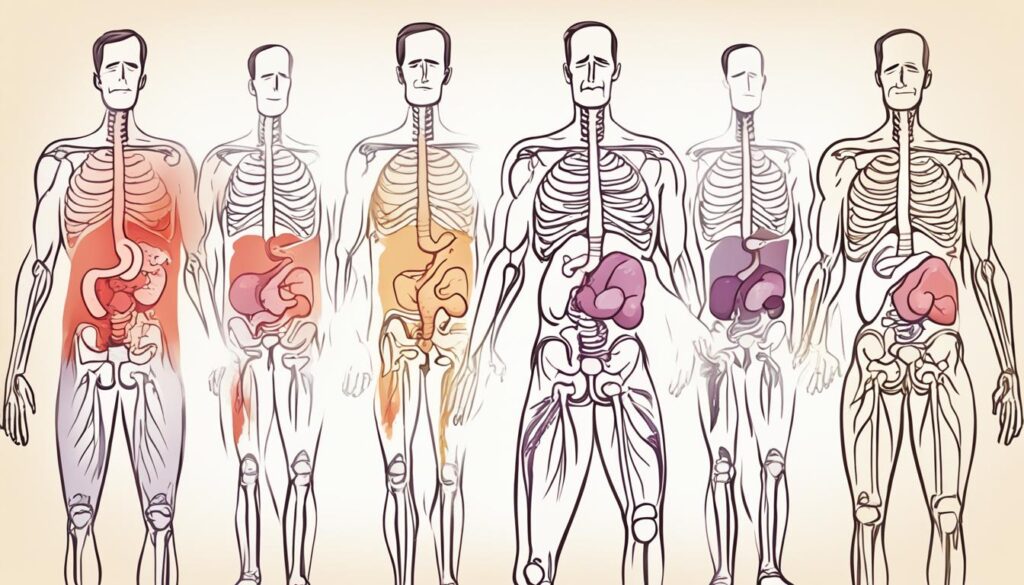
Types of IBD: Crohn’s Disease and Ulcerative Colitis
Crohn’s disease and ulcerative colitis are the main kinds of IBD. Crohn’s can affect any part of the gut, while ulcerative colitis is only in the large intestine and rectum. The places they affect and how they cause swelling are what make these diseases different.
Prevalence and Risk Factors
IBD might affect around 1.6 million Americans, usually before they turn 35. If you have a family history of IBD or are of Jewish descent, your risk goes up. Smoking, certain medicines, and mental health problems can also make IBD more likely.
Crohn’s Disease Explained
Crohn’s disease is a chronic issue that inflames the digestive system. It can happen anywhere from the mouth to the anus. Usually, it affects the end of the small intestine and the colon. The sickness shows up in spots with normal tissue in between.
The sickness can dig deep into the intestinal wall in these patches.
Areas Affected by Crohn’s Disease
Crohn’s can pop up in different parts of the digestive system. But, it’s often found in the end of the small intestine and the colon. This disease makes inflammation spots with healthy areas in between.
This makes it different from ulcerative colitis. That’s because in ulcerative colitis, inflammation spreads continuously.
Symptoms and Complications
People with Crohn’s may experience stomach pain, bloody diarrhea, and lose weight. They might also get a fever and not get enough nutrients. This condition can lead to serious problems like getting blocked, forming unusual openings between organs, or sacks of infection.
There’s also a higher chance of getting colon cancer. But, getting treatments or going into remission might lower this risk.
Ulcerative Colitis Explained
Ulcerative colitis is an inflammatory bowel disease (IBD). It mainly affects the large intestine and rectum. This disease is different from Crohn’s because the inflammation is in one continuous area. It starts in the rectum and moves up into the colon. But it mainly stays in the inner lining of the colon.
Areas Affected by Ulcerative Colitis
This disease causes inflammation in the large intestine and rectum. It usually starts in the rectum. Gradually, it might affect the whole colon. This type of continuous inflammation sets ulcerative colitis apart from Crohn’s disease. Crohn’s can be in different areas of the digestive system in a patchy way.
Symptoms and Complications
People with ulcerative colitis often have diarrhea and rectal bleeding. They may also feel abdominal pain and an urgent need to use the bathroom. The seriousness of these symptoms can vary. Some people might only feel a little uncomfortable. Yet, for others, symptoms can be severe and disrupt their life. In severe cases, it can lead to complications like toxic megacolon and colon wall perforations. These are very serious and need immediate medical attention.

It’s very important to diagnose and treat ulcerative colitis early. This is key to managing symptoms and preventing serious problems in the future. With the right care and lifestyle changes, many people can get their disease under control. They can live a good life with ulcerative colitis.
Causes and Risk Factors of Inflammatory Bowel Disease
Experts don’t fully know what causes inflammatory bowel disease (IBD). They think it’s due to a mix of problems with the immune system, genetic factors, and things in the environment. Knowing about these causes and risks can guide how you and your doctor work together to treat IBD.
Immune System Dysfunction
One major idea is that IBD starts when the immune system goes wrong. In IBD, the immune system attacks the cells in the gut by mistake. This attacking causes swelling and other bad signs. It’s believed to be the main reason we see Crohn’s disease and ulcerative colitis.
Genetic Factors
Our genes also make a big difference in who might get IBD. If you have changes in certain genes, especially in Crohn’s, your chance of getting IBD is higher. If someone in your family has IBD, you have a greater risk too.
Environmental Triggers
Along with problems in the immune system and genes, things in our environment can also set off or make IBD worse. What you eat, how much you stress, if you smoke, and even some medicines might raise your risk of IBD. It’s good to understand what in your environment can trigger IBD signs, so you can try to avoid those things.

Inflammatory Bowel Disease Symptoms
If you have inflammatory bowel disease (IBD), you know the symptoms well. These include stomach pain, diarrhea (sometimes with blood), feeling tired, eating less, and losing weight without trying. The inflammatory bowel disease symptoms can be on and off, with bad times (flare-ups) then better times (remission).
Common Symptoms of IBD
The symptoms of IBD vary but often include:
- Stomach pain and cramps
- Having to go often, with loose or bloody stools
- Feeling tired and not having energy
- Not feeling hungry and losing weight without trying
- Getting a fever
- Feeling sick and throwing up
Extraintestinal Manifestations
IBD might also cause problems outside the stomach, known as extraintestinal manifestations. These can involve:
- Eye problems, like uveitis or episcleritis
- Sores in the mouth called aphthous ulcers
- Red, painful skin lumps like erythema nodosum or pyoderma gangrenosum
- Problems with joints and the back, such as arthritis or ankylosing spondylitis
- Blood flow issues like deep vein thrombosis or pulmonary embolism
- Issues with the liver or kidneys, like primary sclerosing cholangitis
Taking care of your inflammatory bowel disease symptoms is very important. It helps control the disease, stop long-term issues, and make life better.
Diagnosing Inflammatory Bowel Disease
Diagnosing inflammatory bowel disease (IBD) isn’t simple. There’s no one test to spot it. Doctors do several tests to confirm IBD and rule out similar gut issues like irritable bowel syndrome (IBS).
Tests and Procedures
Your doctor might have you undergo various tests and procedures to diagnose IBD:
- Thorough medical history and physical examination
- Colonoscopy with biopsies to examine the lining of the colon and look for signs of inflammation
- Upper endoscopy to inspect the upper digestive tract
- Stool sample analysis to check for signs of bleeding or infection
- Imaging tests, such as X-rays, CT scans, or MRI scans, to provide detailed views of the digestive system and identify any structural abnormalities
- Blood tests to measure inflammation levels and detect IBD-specific biomarkers
Differentiating IBD from IBS
Your doctor needs to tell IBD apart from IBS. Even though they share symptoms, IBD’s cause is chronic gut inflammation while IBS is more about changing bowel habits and discomfort without visible gut issues.
Medical history, symptoms, and test results guide the doctor. Knowing if it’s IBD or IBS helps tailor the right treatment. With the correct diagnosis, your treatment plan can target your symptoms better and boost your well-being.
Inflammatory Bowel Disease and Colon Cancer Risk
If you have inflammatory bowel disease (IBD), especially in a big part of the colon, your risk of colon cancer goes up. Research shows up to four times higher risk of getting colorectal cancer for people with IBD. The longer your bowel stays inflamed, the more likely cancerous changes will happen in the intestine.
Getting IBD at a younger age or having family with colorectal cancer raises your risk even more. If you have IBD, starting around 8-10 years after you’re diagnosed, it’s good to get regular colonoscopies. This helps your doctor find any precancerous changes or cancer early.
Treatment Options for Inflammatory Bowel Disease
There’s no cure yet for inflammatory bowel disease (IBD). However, many treatments can ease symptoms, lower inflammation, and prevent flare-ups. Medication is key, with immunosuppressants, anti-inflammatory drugs, antibiotics, and steroids often prescribed. They target the immune system issues and inflammation.
Medications for IBD
Effective medical plans can keep patients symptom-free for one to three years. The goal is to reduce inflammation, which helps with symptom relief, causes long-term remission, and cuts down on complications.
Surgical Interventions
When medicines aren’t enough, surgery might be necessary. This can involve removing parts of the intestine, fixing blockages or fistulas, or creating a stoma.
Diet and Lifestyle Changes
Changing diet, managing stress, and other lifestyle tweaks can support medical treatments. They play a big role in improving life quality for IBD patients.
Managing Inflammatory Bowel Disease Flare-ups
Living with inflammatory bowel disease (IBD) means facing the challenge of managing flare-ups. A flare-up worsens inflammation in your digestive tract. This results in more diarrhea, pain in the stomach, feeling tired, and other issues. It’s key to tweak your medications, stick to a special diet, and cut down on stress to handle these flare-ups.
Recognizing early signs of a flare and working with your gastroenterologist are crucial. This can make flare-ups less severe and shorter. Keeping in touch with your healthcare team and monitoring your health helps. It allows you to act early in handling managing IBD flare-ups and keep your well-being in check.
During a flare-up, you might need to change your medicine. You could have to take more anti-inflammatory or immunosuppressant drugs for a while. Your doctor might also suggest trying other medications. These steps aim to help better manage the inflammation and relieve your symptoms.
Along with medications, a special diet can be useful. You might have to stop eating high-fiber foods, dairy, or others that make your symptoms worse. Keeping a food diary is handy. It lets you figure out and avoid foods that might trigger a flare-up.
Managing your stress and lowering anxiety are also vital in preventing flare-ups. Things like meditation, deep breathing, or light exercise can help. They make it easier to deal with the stress of having IBD. This can make a big difference in your health.
By spotting IBD flare signs early and making changes to your treatment, you can act and get better. Also, using stress management techniques matters. This way, you become an active part of managing IBD flare-ups and lessen how much they disrupt your life.
Living with Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) brings physical, emotional, and social hurdles. But, managing it right with support helps keep life good. IBD can make people feel judged, affecting their happiness. Working can be hard due to symptom management issues and lack of workplace support.
Coping Strategies
Knowing how to cope is key for those with IBD. Strategies like meditation or joining a group can reduce stress. A good diet, staying active, and enough sleep can also ease IBD symptoms. And, working with a doctor to find the best treatment plan is crucial.
Support Resources
Turning to family, friends, or IBD groups can be a great help. They offer both emotional and practical advice. Mental health resources and support for issues like anxiety are also available. Healthcare providers can help point out these resources.
By looking after your body and mind, and using available support, dealing with IBD becomes more manageable. This way, you can keep living a rich life despite the condition’s challenges.
Inflammatory Bowel Disease in Children
Inflammatory bowel disease, or IBD, impacts not just adults but also children. Teenagers get diagnosed more than younger kids. Spotting the disease in children, especially older ones, can be tricky. Yet, it’s vital to catch it early and treat it right. Doing so is key because IBD can greatly affect children’s growth and life quality.
Children with IBD might need more than usual medical treatments. They could benefit from special diets, mental health support, and a close watch by a team of healthcare experts. This wider care plan is crafted to meet the specific needs of kids with IBD.
Here are some facts on IBD in children:
- The incidence rate of pediatric IBD in Northern California was between 233-239 per 1,000 kids from 1996 to 2006.
- The prevalence rate of pediatric IBD in Wisconsin was about 19 cases per 100,000 kids.
- 143 per 100,000 children were newly diagnosed with IBD in Wisconsin.
- The prevalence of Crohn’s disease and ulcerative colitis in a US insured population was seen at 58 cases per 100,000.
Several things, like genes and where you live, can affect a child’s IBD risk. Being born through a C-section could raise this risk by 1.8 times. However, breastfeeding might cut the risk by 20%. Using antibiotics in the first year of life is another risk factor.
Parents who work closely with their child’s gastroenterologist and medical team can help a lot. By ensuring their child gets the right care, these parents can help their child with IBD lead a normal, happy life.
Research and Developments in IBD
Scientists are diving deep into the world of IBD research. Their aim is to create better treatments and perhaps, one day, find a cure. They are studying how the gut’s bacteria, your genes, and issues with the immune system play a role in getting and worsening IBD. Excitingly, new medicines like biologics that target certain inflammation paths are doing well in tests for Crohn’s disease and ulcerative colitis.
Moreover, progress in IBD research and surgeries is changing the game for patients needing operations. Techniques that are less invasive are making recovery easier. As we learn more about IBD, patients can expect more tailor-made and creative solutions to live better with this long-term illness.
Conclusion
Inflammatory bowel disease is a complex, long-term condition. It can really affect your life. There is no cure yet for inflammatory bowel disease. But, thanks to more knowledge and better treatments, doctors can help manage Crohn’s disease and ulcerative colitis. Working closely with a gastroenterologist, living healthily, and using support resources can help you control the disease. This way, you can stay well.
With ongoing research, there’s hope for better ways to handle and maybe even cure inflammatory bowel disease. By being proactive and seeking the right support, those with inflammatory bowel disease can lead healthy lives. They can learn to manage the disease and still enjoy good quality of life.
FAQ
What is inflammatory bowel disease (IBD)?
IBD is a long-term disorder of the digestive system. Its main types are Crohn’s disease and ulcerative colitis. Both affect the colon, rectum, and sometimes other areas.
What are the symptoms of inflammatory bowel disease?
The main signs are stomach pain, diarrhea (sometimes bloody), and feeling very tired. You might also lose weight without trying. IBD can lead to problems elsewhere in the body, too.
How is inflammatory bowel disease diagnosed?
Diagnosing IBD involves many tests. These include a detailed medical history, a physical check-up, and procedures like colonoscopy. Doctors might also check your stool, use imaging tests, and more.
What are the treatment options for inflammatory bowel disease?
Medicines are key in managing IBD. Doctors use drugs that ease inflammation and control the immune system. In some cases, surgery might be needed.
How can I manage inflammatory bowel disease flare-ups?
To handle flare-ups, your doctor might change your medicines. You also need to watch your diet and manage stress. Acting fast and working closely with your gastroenterologist is important.
Does inflammatory bowel disease increase the risk of colon cancer?
Yes, IBD, especially when it affects a large area of the colon, raises colon cancer risk. It’s crucial for IBD patients to have regular colonoscopies. This check can spot cancer early or find precancerous changes.
Can children develop inflammatory bowel disease?
IBD is not just for adults; children can get it too, mostly in their teenage years. It’s vital to diagnose and treat IBD early in kids. The disease can affect their growth and quality of life.
What are the latest developments in inflammatory bowel disease research?
Scientists are making progress in understanding IBD. They aim to find better treatments and maybe a cure. They’re looking at the role of the gut’s bacteria, genes, and immune issues in IBD.
Source Links
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/inflammatory-bowel-disease
- https://www.mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/symptoms-causes/syc-20353315
- https://www.ncbi.nlm.nih.gov/books/NBK470312/
- https://www.healthpartners.com/blog/understanding-ibd/
- https://www.niddk.nih.gov/health-information/digestive-diseases/crohns-disease/definition-facts
- https://www.mayoclinic.org/diseases-conditions/crohns-disease/symptoms-causes/syc-20353304
- https://medlineplus.gov/crohnsdisease.html
- https://www.niddk.nih.gov/health-information/digestive-diseases/ulcerative-colitis
- https://www.mayoclinic.org/diseases-conditions/ulcerative-colitis/symptoms-causes/syc-20353326
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2886488/
- https://www.mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/diagnosis-treatment/drc-20353320
- https://nyulangone.org/conditions/inflammatory-bowel-disease/diagnosis
- https://www.crohnscolitisfoundation.org/patientsandcaregivers/what-is-ibd/diagnosing-ibd
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10452690/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9913122/
- https://acripc.com/managing-symptoms–flares-of-inflammatory-bowel-disease.htm
- https://www.crohnscolitisfoundation.org/patientsandcaregivers/mental-health/navigating-daily-life-with-ibd
- https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/lifestyle-and-diet-in-inflammatory-bowel-disease
- https://www.webmd.com/ibd-crohns-disease/features/ibd-wish-you-knew
- https://www.childrenshospital.org/conditions/inflammatory-bowel-disease
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4702263/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10382792/


