If you’re dealing with GERD (Gastroesophageal Reflux Disease) and back pain, you’re not alone. This condition makes stomach acid flow back into the esophagus, causing back pain. But, there’s hope. This guide will show you ways to manage your GERD back pain and find relief.
Table of Contents
ToggleWe’ll look at lifestyle changes, medicines, and other treatments for GERD back pain. By trying different approaches, you can ease your pain and improve your life. Let’s help you take back your active, pain-free life.
Understanding GERD and Its Connection to Back Pain
Gastroesophageal reflux disease (GERD) is a common digestive issue that affects your health, including your back. It happens when the valve between your stomach and esophagus gets weak or relaxed. This lets stomach acid flow back into your esophagus, causing symptoms like heartburn and difficulty swallowing.
What is GERD?
GERD is a long-term condition that can make the esophagus lining inflamed and irritated. This can damage the esophagus over time. It also raises the risk of serious issues, such as ulcers or Barrett’s esophagus, which is a condition that could lead to cancer.
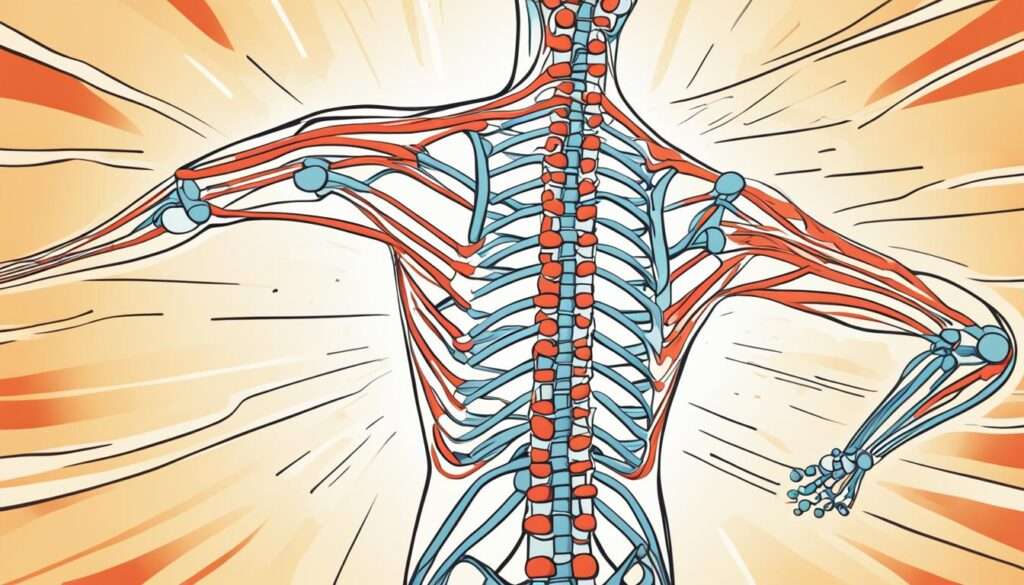
How GERD Causes Back Pain
GERD and back pain are linked because the esophagus and spine are close together. When stomach acid flows back into the esophagus, it can irritate the nerves and muscles in the back. This leads to discomfort and pain. The pressure from stomach contents on the esophagus can also cause pain in the back.
GERD can cause different types of back pain, including:
- Dull, aching pain in the upper or middle back
- Burning sensation in the back that may radiate to the shoulders or neck
- Difficulty with certain movements or positions that make the pain worse
Knowing how GERD and back pain are connected is key to finding ways to ease your pain and improve your life.
Lifestyle Modifications for GERD Back Pain Relief
Making changes in your life can help ease GERD-related back pain. Focus on eating better, managing your weight, and avoiding certain foods. These steps can lessen the number and intensity of reflux episodes, helping your back feel better.
Dietary Changes
Choosing the right foods is key. Stay away from fatty, spicy, and acidic foods as they can make reflux worse and hurt your back. Go for a diet full of lean proteins, whole grains, and fruits and veggies that aren’t citrus.
Weight Management
Keeping a healthy weight is important for controlling GERD and back pain. Being overweight puts extra pressure on the esophageal sphincter, making acid reflux more likely. Losing weight can ease this pressure and help your back.
Avoiding Triggers
Some foods and drinks can make GERD and back pain worse. Avoid things like caffeine, alcohol, and fizzy drinks. They can relax the esophageal sphincter and cause acid to flow back up.
By making these lifestyle changes, you can take charge of your GERD-related back pain. This can greatly improve your health and well-being.
Medications for GERD Back Pain Management
Alongside lifestyle changes, many [GERD medications] can help manage GERD-related back pain. [Over-the-counter treatments] like Tums or Rolaids can quickly ease symptoms by neutralizing stomach acid. [Prescription drugs], such as H2 blockers (e.g., ranitidine) and proton pump inhibitors (e.g., omeprazole), cut down acid production and protect the esophagus. Together with lifestyle changes, these treatments can lessen GERD symptoms and back pain.
Over-the-counter antacids are great for fast relief from GERD back pain. They neutralize stomach acid, offering quick relief from the burning and discomfort. Prescription medications tackle the root causes of GERD by lowering acid levels and healing the esophageal lining. These medications are key to a full treatment plan for GERD and back pain.

It’s crucial to work closely with your healthcare provider to find the right [GERD medications] for you. They can guide you through the different options and make sure you’re using them safely and effectively. This ensures the best results for your GERD-related back pain.
Complementary and Alternative Therapies
If you’re dealing with back pain from gastroesophageal reflux disease (GERD), you might want to try complementary and alternative therapies. These natural methods can help along with traditional treatments. They aim to address the root causes of GERD.
Herbal Remedies for GERD
Herbal remedies can ease inflammation and cut down on acid production. This can help reduce GERD symptoms, including back pain. Ginger is known for its anti-inflammatory effects and can soothe the digestive system.
Chamomile and licorice root are also popular for their calming effects on the esophagus. You can try these herbal remedies for GERD and see if they help you feel better.
Acupuncture for GERD
Acupuncture is another option that might help with GERD. It’s a traditional Chinese medicine that uses thin needles to relax and improve digestion. Research shows acupuncture could ease GERD symptoms, including back pain, by balancing the body’s natural processes.
If you’re interested in acupuncture for GERD, look for a licensed practitioner near you.
Though the science on these treatments is still growing, they might offer extra relief for some with GERD-related back pain. Always talk to your healthcare provider before trying new therapies.

Identifying and Treating Underlying Causes
Dealing with ongoing GERD-related back pain means finding and fixing any underlying issues. Conditions like hiatal hernia and esophageal strictures can make GERD worse and cause back pain.
Hiatal Hernia
A hiatal hernia happens when part of the stomach moves up into the chest through the diaphragm. This can make acid reflux worse since stomach contents can flow back into the esophagus more easily. Fixing a hiatal hernia can help stop the GERD-related back pain.
Esophageal Strictures
Esophageal strictures narrow the esophagus, making it hard for food and stomach acid to move through. This can cause reflux and back pain. Treating these strictures, often with surgery, can help people with long-term GERD-related back pain.
Addressing these causes can help you manage your GERD-related back pain better. Working with your healthcare provider to create a full treatment plan is key. This plan should tackle both symptoms and the underlying causes of your condition.
GERD Back Pain
If you’re dealing with ongoing back pain, it might be linked to your GERD (Gastroesophageal Reflux Disease). GERD is a common digestive issue that can affect your health, including causing back pain.
Stomach acid flowing back into your esophagus can irritate your back’s nerves and muscles. This leads to discomfort and pain. It’s important to understand how GERD and back pain are connected to get the right treatment and relief.
Symptoms of GERD-Related Back Pain
- Dull, aching pain in the upper or middle back
- Worsening of back pain after meals or when lying down
- Difficulty sleeping due to back pain
- Burning sensations in the back or chest
- Difficulty swallowing or feeling of a lump in the throat
Causes of GERD-Related Back Pain
- Acid reflux: The backflow of stomach acid into the esophagus can irritate the nerves and muscles in the back, leading to pain.
- Hiatal hernia: A condition where the stomach protrudes through the diaphragm, which can contribute to GERD and back pain.
- Esophageal spasms: Involuntary contractions of the esophageal muscles can cause pain that may radiate to the back.
If you’re facing back pain due to GERD, it’s crucial to see a doctor. They can help find the cause and create a treatment plan. This might include changes in your lifestyle, medications, or even surgery to ease your symptoms and bring relief.

Exercise and Physical Therapy for Back Pain Relief
Dealing with back pain from GERD needs a mix of approaches. Adding exercises and physical therapy can really help. By doing low-impact workouts and specific exercises, you can ease the pain and feel better overall.
Low-Impact Exercises
For GERD back pain, pick low-impact activities that don’t make things worse. Walking, swimming, and cycling are great choices. They work the back muscles gently and don’t strain the body too much. These exercises boost circulation, strengthen the core, and increase mobility. They also lower the chance of making GERD worse.
Stretching and Strengthening Exercises
Along with low-impact exercises, certain stretches and strengthening moves can help. They focus on the back and core muscles. This can ease the strain on the esophagus and back, reducing GERD-related back pain. Think about doing gentle back stretches, core-strengthening planks, and exercises like cat-cow poses. A physical therapist can create a plan just for you and your GERD symptoms.
Adding exercises for GERD back pain, physical therapy, and low-impact workouts to your routine is a big step. It helps manage your GERD-related back pain and improves your life quality.

Managing Stress and Anxiety
Stress and anxiety can make GERD symptoms worse, including back pain from reflux. It’s key to tackle these feelings to help your back pain.
Using stress management techniques can lessen the effects of GERD. Meditation, deep breathing exercises, and mindfulness help you relax. These can reduce your reflux symptoms and ease your back pain.
Try other ways to handle stress and anxiety, such as:
- Regular exercise to release endorphins and manage stress
- Journaling or expressive writing to process emotions
- Engaging in hobbies or activities you enjoy to find balance
- Seeking support from friends, family, or a mental health professional
By managing your stress and anxiety, you can lessen GERD’s effects and ease your back pain. It’s important to find relaxation techniques that suit you and use them daily for the best results.
Posture and Ergonomic Adjustments
Keeping a good posture and making your workspace ergonomic can help with GERD-related back pain. Make sure your spine is straight, shoulders back, and head up. This reduces back strain and pressure on your esophagus.
Using a standing desk is a good idea. Standing desks help ease the discomfort of sitting too long and improve posture. Also, adding lumbar support to your chair keeps your spine’s natural curve. This stops slouching and lowers back pain.
Don’t forget about your computer screen’s height and position. Keep the screen at eye level to avoid neck strain and promote good posture. A document holder next to your computer also helps keep your head and neck in a neutral position. This lowers the risk of GERD back pain.
With these posture correction and ergonomic adjustments, you can ease GERD back pain and boost your health.
When to Seek Medical Attention
If you’re dealing with ongoing or getting worse GERD-related back pain, it’s key to get medical help. There are signs that show you need more checks and maybe treatment.
Warning Signs
- Persistent or recurrent heartburn, acid reflux, or regurgitation
- Difficulty swallowing or feeling of food stuck in the throat
- Unexplained weight loss
- Severe or sudden chest pain
- Persistent hoarseness or sore throat
These symptoms might mean you have a condition that needs a doctor’s care. If you notice any of these GERD warning signs, don’t wait to talk to your healthcare provider.
Diagnostic Tests
Your doctor might suggest some tests to figure out why your back hurts from GERD. These tests could be:
- Endoscopy: This lets your doctor look at your upper digestive tract for any problems or damage.
- pH monitoring: This test checks how much acid is in your esophagus to find out what’s causing your symptoms.
- Imaging studies: X-rays, CT scans, or MRI scans can show your digestive system and find any hidden issues.
These diagnostic tests help your doctor make a plan to help with your GERD back pain. If your symptoms keep up or get worse, don’t delay in seeing a doctor for GERD.
Surgical Options for Severe Cases
If you’re dealing with severe GERD-related back pain and other treatments haven’t helped, surgery might be an option. Your doctor may suggest surgery to fix the root cause of GERD and ease your back pain.
Fundoplication is a common surgery for GERD. It strengthens the muscle at the bottom of the esophagus. This muscle stops acid from flowing back up, helping to reduce back pain and other GERD symptoms.
For people who are overweight or obese, bariatric surgery might be suggested. These surgeries can help manage GERD by addressing weight issues. They offer long-term relief from back pain and other symptoms.
Remember, surgery has risks like infection, bleeding, and trouble swallowing. Your doctor will look at your situation closely. They’ll talk about the good and bad sides of each surgery before making a suggestion.
If your back pain from GERD is bad and other treatments didn’t work, talk to a healthcare expert. They can guide you on surgical options that might be right for you. With the right care, you can find relief and manage your GERD better.
Preventing GERD Back Pain Flare-Ups
Managing your GERD well is key to avoiding back pain. Keep an eye on your triggers and live a healthy life. This way, you can reduce reflux-related discomfort.
Monitoring Triggers
First, find and avoid your GERD triggers. Watch how your body reacts to certain foods, drinks, and habits. Common triggers include:
- Spicy, fried, or acidic foods
- Caffeinated drinks, alcohol, and carbonated beverages
- Eating large, heavy meals close to bedtime
- Lying down immediately after eating
- Excess weight and tight-fitting clothing
- High-stress levels and poor sleep habits
Use a food and symptom diary to find your triggers. Then, adjust your diet and lifestyle as needed.
Maintaining a Healthy Lifestyle
Healthy habits help prevent GERD back pain. Add these to your daily life:
- Eat a balanced, GERD-friendly diet rich in fruits, vegetables, and whole grains.
- Maintain a healthy weight through regular exercise and portion control.
- Practice stress management techniques, such as meditation, yoga, or deep breathing.
- Establish a consistent sleep schedule and aim for 7-9 hours of quality sleep each night.
- Quit smoking and limit your alcohol intake, as these can worsen GERD symptoms.
By watching your triggers and living healthily, you can prevent GERD back pain flare-ups.
Coping Strategies for Chronic GERD Back Pain
Living with chronic GERD-related back pain is tough, but you can manage it. There are strategies that help with both the physical and emotional sides. By using a full approach, you can feel better and live better.
Pain Management Techniques
Trying different pain management techniques can really help. Do relaxation exercises like deep breathing, meditation, or yoga to ease muscle tension and stress. Using heat or cold on the sore spots can also bring relief. And, if needed, over-the-counter pain meds can help with the pain.
Emotional Support
GERD can affect your feelings too. Getting support from friends, family, or a support group is key. Talking with others who know what you’re going through can make you feel less alone.
Dealing with GERD back pain is complex. Use pain management and emotional support together to tackle it. Keep going, and don’t be afraid to get professional help if you need it.
Conclusion
Managing GERD-related back pain means using a full approach. This includes changing your lifestyle, managing your meds, and sometimes surgery. By fixing the root causes and using proven treatments, you can ease your pain and better your life.
Understanding how GERD and back pain are linked helps you find the right treatments. You can try diet changes, manage your weight, and use other therapies. This article has shown you ways to handle GERD back pain and get better.
With the right treatments and a focus on your health, you can beat GERD back pain. Keep an eye on your health, work with your doctors, and look into new ways to manage GERD back pain. This way, you can live a life without pain.
FAQ
What is GERD?
GERD stands for Gastroesophageal Reflux Disease. It’s a condition where stomach acid flows back into the esophagus. This can cause severe heartburn and other symptoms.
How does GERD cause back pain?
When stomach acid flows back into the esophagus, it can irritate the nerves and muscles in the back. This irritation leads to discomfort and pain.
What dietary changes can help manage GERD-related back pain?
Eating fewer fatty, spicy, and acidic foods helps. Avoiding caffeine, alcohol, and carbonated drinks also reduces reflux episodes.
What medications are available for GERD back pain management?
There are over-the-counter antacids, H2 blockers, and proton pump inhibitors. These medications reduce acid production and protect the esophagus.
How can complementary and alternative therapies help with GERD back pain?
Herbal remedies like ginger, chamomile, and licorice root, and acupuncture may help some people with GERD back pain.
When should someone seek medical attention for GERD back pain?
See a doctor if symptoms don’t go away or get worse, if swallowing is hard, or if you lose weight without trying. These could mean you need more treatment.
What are the surgical options for severe GERD-related back pain?
For severe cases, surgery like fundoplication or bariatric surgery might be needed. These surgeries aim to fix the root causes of GERD.
How can exercise and physical therapy help manage GERD back pain?
Doing low-impact exercises and specific stretches can help. They improve mobility, strengthen muscles, and ease strain on the esophagus and back.
What role does stress and anxiety play in GERD back pain?
Stress and anxiety can make GERD symptoms worse, including back pain. Managing stress can lessen the effects of GERD.
How can proper posture and ergonomic adjustments help with GERD back pain?
Good posture and ergonomic changes can ease back strain and reduce pressure on the esophagus. This helps manage GERD back pain.
Source Links


